Paul Cowling MSc FRCS (Tr & Orth)
Consultant Trauma and Orthopaedic Surgeon
Specialist interest in Upper Limb Surgery
Leeds Teaching Hospitals NHS Trust
(Richard Montgomery MB BS FRCS FRCSEd, (Honorary Consultant in Trauma & Orthopaedic Surgery, South Tees NHS Trust & Newcastle upon Tyne Hospitals NHS Trust) apologises for introducing any typos & errors of transcription; they are his alone).
Background
Clavicle fractures are common upper limb injuries, accounting for approximately 35% of injuries to the shoulder girdle, and of these, fractures of the shaft contribute the majority (69-82%).
Lateral/distal clavicle fractures, due to their proximity to the acromioclavicular joint and involvement with the coraco-clavicular ligaments, are classified and treated with a different philosophy to a midshaft clavicle fracture. They should be regarded as an entirely different injury. They account for 21-28% of clavicle fractures.
Lateral fractures and clavicle fractures in children will be the subjects of separate articles in due course.
Clavicle fractures most commonly occur in males aged <30 years. The injury often occurs due to sporting activity, when a fall occurs, and due to inertia, a patient is thrown forwards landing on an unprotected shoulder. This is a common occurrence in cyclists & equestrians. Another peak in incidence occurs in the elderly (often >80 years), with slight female predominance. These injuries are more associated with low energy falls from a standing height, and are related to osteoporosis.
Handy references for a general overview of mid-shaft clavicle fractures and their epidemiology include:
Robinson CM. ‘Fractures of the clavicle in the adult. Epidemiology and classification’. J Bone Joint Surg Br 1998; 80: 476-484
Postacchini F, Gumina S, De Santis P, ALbo F. ‘Epidemiology of clavicle fractures’. J Shoulder Elbow Surg 2002; 11: 452-6
Khan et al. ‘Fractures of the clavicle’. J Bone Joint Surg Am. 2009; 91: 447-460.
Functional and radiological outcomes
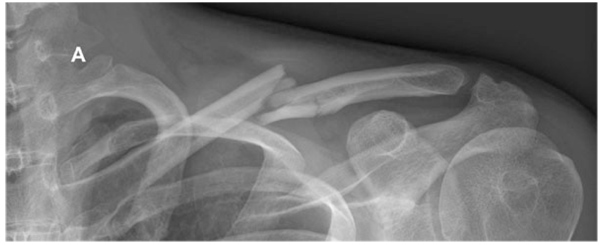
Historically, almost all midshaft clavicle fractures were treated non-operatively, with the exception of open fractures, fractures with a neurovascular compromise, or in the situation of a ‘floating shoulder’ (a fracture of the clavicle and the scapular neck).
Canadian Orthopaedic Trauma Society. ‘Nonoperative treatment compared with plate fixation of displaced midshaft claviclar fractures: a multicenter, randomized clinical trial’. JBJS Am 2007; 89: 1-10
Plate fixation and non-operative treatment have both shown an improvement in outcome over time. This Canadian study found that patients in both groups improved their Constant score and DASH score up to a year following injury, with the operative group demonstrating higher scores at that point. However, in the operative group, complications of wound infection and subsequent metalwork removal occurred; in the non-operative group, 18% went on to nonunion, and thus required surgical management anyway.
Subsequent randomised controlled trials (RCT) between fixation Vs non-operative management of displaced midshaft clavicle fractures have also demonstrated a non-union rate of 11-23.1% in non-operatively managed fractures.
These RCTs showed no difference in DASH or Constant scores between the two groups at the longest follow-up, which ranged from 9 -12 months. Generally, amongst both op/non-op clavicle fractures, Constant scores had recovered to >91 and DASH to <4.55-7 by the time of the latest follow-up.
The references for these RCTs on clavicle fracture fixation Vs non-operative management are as follows:
Woltz S et al. ‘Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures’. JBJS Am 2017 99; 2: 106-112
Ahrens PM et al. ‘The Clavicle trial: a multicenter randomized controlled trial comparing operative with nonoperative treatment of displaced midshaft clavicle fractures’. JBJS Am. 2017 99; 16: 135-154
Qvist et al. ‘Plate fixation compared with nonoperative treatment of displaced midshaft clavicle fractures: a randomised controlled trial’. Bone Joint J 2018 100; 10: 1385-1391
Operative management of clavicle fractures is associated with a number of problems & complications that have the subject of systematic review:
Wijdicks et al, ‘Systematic review of the complications of plate fixation of clavicle fractures’.Arch Orthop Trauma Surg (2012) 132:617–625 DOI 10.1007/s00402-011-1456-5
These are infection, fixation irritation, fixation failure, need for subsequent removal, nonunion, refracture after removal. Neurovascular & lung complications are thankfully rare.
The effect of a malunited clavicle on outcome
One of the concerns previously discussed in the literature was that conservatively managed fractures might well go on to heal in the majority of cases, but they would do so with some shortening of the clavicle.
Goudie et al. ‘The influence of shortening on clinical outcome in healed displaced midshaft clavicular fractures after nonoperative treatment’. JBJS Am 2017; 99: 1166-1172.
This study from Edinburgh investigated patients using CT scans of both clavicles to determine the amount of shortening in 48 patients. The mean shortening was measured at 11.3mm, and the degree of shortening did not correlate with DASH, Constant or SF-12 scores at any point during follow-up, up to 1 year following injury. On investigating those with the most shortening (2cm or more), again no correlation with functional outcome was found.
Malik et al. ‘Is shortening of displaced midshaft clavicle fractures associated with inferior clinical outcomes following nonoperative management: A systematic review’. J Shoulder Elbow Surg 2019; 28: 1626-1638.
This recent review article into the effect of shortening also demonstrated no significant association with either nonunion rates, or shoulder outcome scores in displaced midshaft clavicles managed non-operatively.
McKee et al. ‘Deficits following nonoperative treatment of displaced midshaft clavicular fractures’. JBJS Am 88; 1: 35-40
Functional deficits related to healed non-operatively treated clavicle fractures have been investigated. This small study from Canada tested function at a mean of 55 months following clavicle fracture. They demonstrated that their 30 patients under review had maintained reasonable range of movement of mean flexion to 170 deg, & mean abduction to 165 deg. Strength, compared to the contralateral uninjured shoulder, was reduced to 81% for flexion, 75% for endurance in flexion, 82% for abduction. Mean Constant score was 71 points, and mean DASH was 24.6 points.
Long-term effects
Shapira S. et al. ‘Effect of malunited midshaft clavicular fractures on shoulder function’. ISRN Orthopaedics Vol 2011 Article ID 507287 5 pages.
Shapira et al examined 25 patients at a mean of 38 months following clavicle fracture treated with nonoperative management. They found that range of motion was preserved, demonstrating <6% difference to the contra-lateral uninjured side. In addition, there was a reduction in abduction strength of the affected shoulder of 7%.
Hillen et al. ‘Long term follow-up of conservatively treated midshaft clavicular fractures on functional outcome’. J Orthop 2019 11; 18: 80-85
This series of 18 patients was reviewed at mean follow-up time of 13.5yrs following non-operative management of mid-shaft clavicle fracture. No difference in strength was noted between injured and unaffected side.
Chalidis B et al. ‘Acute management of clavicle fractures: A long term functional outcome study’. Acta Orthop. Belg. 2008; 74: 303-307
This large case series of 139 patients looked at outcomes of all clavicle fracture treatment options at a mean of 7 .2 years. The vast majority (124) were managed without surgery, with 97% going on to unite. Despite fracture union, just under one third of patients reported mild pain or discomfort with overhead activities. However, it is worth noting this study did include all types of clavicle fracture, not just midshaft injuries.
George et al. ‘The long-term outcome of displaced mid-third clavicle fractures on scapular and shoulder function: variations between immediate surgery, delayed surgery, and nonsurgical management’. JSES 2015 24; 669-676
George et al retrospectively analysed 3 groups of 20 patients who underwent midshaft clavicle fracture fixation (mean 5.2yrs follow-up); delayed fixation (6.27yrs follow-up); and non-operative management (mean 4.3yrs follow-up).
The conservatively managed group demonstrated the best DASH and ASES functional scores, but this group also recorded the biggest decrease in range of movement, which seemed to correlate with the greater amounts of clavicular shortening.
Clavicle fractures with concurrent injuries
George et al (vide supra) also found that if another concurrent injury was sustained, Constant scores were lower than an isolated clavicle fracture.
Ferree S et al. ‘Comparing fracture healing disorders and long-term functional outcome of polytrauma patients and patients with an isolated displaced midshaft clavicle fracture’. JSES 2017; 26: 42-48
This study retrospectively compared two groups of patients: those with polytrauma and a clavicle fracture, and those with an isolated displaced midshaft clavicle fracture. They found a similar rate of nonunion between the groups, but the polytrauma patients demonstrated a worse functional outcome using the Quick DASH measure.
Nonunion/Malunion surgery outcomes
When nonoperative management fails to achieve union, some patients elect for surgery to attempt to achieve union of their mid-shaft clavicle fracture. There is little in the literature investigating the outcomes on surgery for nonunion/malunion.
Kluijfhout WP. ‘Plate fixation of clavicle fractures: comparison between early and delayed surgery’. JSES 2020 29; 266-272
This Dutch study compared the outcome of nonunion surgery (delayed surgery) to early surgery. Although the criteria for establishing a nonunion were not documented, the median time to surgery for the nonunion patients was 162 days in 48 patients. These patients were compared to 73 patients undergoing surgery acutely at median 7 days following injury. Delayed surgery was associated with a higher risk of complications, but functional outcomes were reasonable. However, these functional outcomes remained inferior to those undergoing acute surgery when assessing mean DASH (5.4 for acute fixation Vs 15.1 in delayed surgery), and Constant score (96.2 Vs 84.4). It is worth noting, however, that this study’s outcomes were recorded at ‘at least 6 weeks following surgery’, so long-term comparisons cannot be taken from this study. Since other authors have shown that these injuries continue to improve for far longer than this, this represents a considerable methodological weakness.
Strong DH. ‘Operative management of clavicular malunion in midshaft clavicular fractures: a report of 59 cases’. JSES 2019; 28: 2343-2349
This recent paper from Australia examined 59 cases who had undergone operative management of a clavicle malunion that had initially been treated nonoperatively. The indications for surgery were pain, impaired function, scapular prominence, rotator cuff pain, cosmetic deformity or a ‘sensation that the shoulder did not feel right’. The authors found that a corrective osteotomy with the aim to restore length and alignment provided a DASH score of 1.81 at mean 12 months following surgery. Though 2 patients did develop infection requiring revision fixation, union was subsequently achieved. A further 2 patients had fractures adjacent to their metalwork after union was achieved.
It is reassuring that malunion following non-operative management can still be retrieved subsequently, in the small number that require intervention.
Summary
Most surgeons agree that operation is required for open fractures, fractures with a neurovascular compromise, or in the situation of a ‘floating shoulder’ (a fracture of the clavicle and the scapular neck).
Non-operative management is associated with nonunion rates of ~11%-23%
Operative management is associated with infection rates of <10% in all but 2 studies , non-union of <10%. Metalware removal because of prominence is required in 10%-64% (!); refracture can follow in between 1%-5%.
The outcome scores of op/non-op are not greatly dissimilar. Studies show a variable degree of weakness or loss of range of motion after midshaft clavicle fracture. If function is affected, it tends to be in activities above shoulder level.
Malunion of the clavicle does not seem to be associated with any significant outcome score deficit. If thought necessary, secondary surgery can usually retrieve the situation.