Tibial plateau fractures (TPF) illustrate the concept of ‘fracture personality’ very well. They range from the invisible occult fracture (where the only challenge is diagnosis), right through to a technically-challenging multi-fragmentary nightmare that will give you almost as many flashbacks as the poor patient.
I’ll start with occult TPFs. These usually present after relatively minor trauma as a painful joint with an effusion, which may be a small effusion to start with. The amount of trauma necessary to cause the fracture is proportionate to bone quality; perhaps a tackle in a young footballer, a fall from standing height in a grandmother. The patient may be able to partially weight bear through the limb, but usually not fully, and not for long. (Bear in mind the analgesic effect of alcohol or other unofficial or official medications).
Kiel et al. BMC Musculoskeletal Disorders (2018) 19:244
https://doi.org/10.1186/s12891-018-2170-z. These authors reviewed 137 patients with delayed diagnosis of a fracture within the knee after trauma, to see if using the Pittsburgh Knee Rules (PKRs) could have reduced the number of TPFs that went undiagnosed. Only 42% had been evaluated using the PKRs. In 53 cases the fracture had not been diagnosed on radiographs, even though in 84% of these the fracture was visible or suspected in retrospect. 50 of 79 patients in whom X-ray was not done, were in fact candidates for X-ray according to the rules.
Unfortunately, in 53% of these missed cases, fracture position had worsened by the time of diagnosis; a significant disability compensation was granted in 36% of cases due to delayed diagnosis (totalling 841,000 euros).
I shall briefly digress onto the Pittsburgh Knee Rules, formulated by Dr Seaberg. The rules suggest X-ray after a blunt trauma or fall if: age <12 or >50; & the patient is unable to take 4 full weight-bearing steps on a flat foot.
Tank et al, 2013 (DOI:https://doi.org/10.1016/j.ajem.2012.11.003) found the PKR to be equally sensitive to the Ottawa Knee Rules (0.86), but more specific at 0.51, versus 0.27 for the OKR.
As always, with occult tibial fractures, the key to diagnosis is suspicion. If the X-ray is negative, but you seriously suspect fracture, consider MRI.
Being naturally a ‘lumper’ rather than a ‘splitter’ as far as classifications are concerned, I prefer a classification that is:
-simple (memorable!)
– reproducible (high kappa)
– relevant to treatment AND prognosis
-represents a lingua franca for most orthopaedic surgeons.
There is a plethora of PTF classifications. Most do not tick enough of the boxes above as far as I’m concerned, and I’m going to mention just a few. I think the ones that follow are the best-known and most useful when planning treatment. To what extent they affect prognosis is a moot point.
Palmer (1951, JBJS, VOL. 33 B, NO. 2, May 1951, p160-166) classified these injuries into split, depression, and T or Y fractures. n=98. Unsurprisingly, the split or mildly comminuted cases had the best results; the ones whose articular surfaces had been rendered into a mosaic of small fragments did worst. He did not find any effect of age. Nearly half regained normal or near-normal range of motion.
Schatzker developed these ideas and came up with a 6-type classification system that is widely used (Shatzker J ‘Compression in the surgical treatment of fractures of the tibia’. CORR No 105, Nov-Dec 1974 220-239).

AO/OTA developed a classification that is apparently more reliable in terms of intra- and inter- observer reliability than Shatzker’s classification (Walton et al 2003. ‘AO or Schatzker? How reliable is classification of tibial plateau fractures?’. Arch Orthop Trauma Surg 123, 396–398 (2003). https://doi.org/10.1007/s00402-003-0573-1).
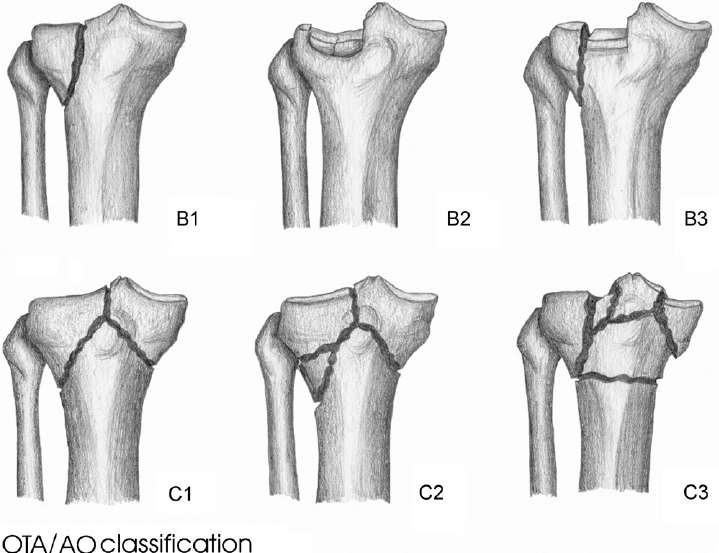
The progress of B unicondylars through split/depression/split-depression seems logical and related to both treatment & likely prognosis (or maybe not – as later papers* suggest!). Likewise bicondylar Cs from simple/metaphyseal comminution/metaphyseal and articular comminution seems appropriate. My preferred classification.
Another problem with X-ray classifications is that they reinforce an orthopaedic surgeon’s natural tendency to think and treat in X-ray terms, ignoring the associated soft tissue injury. TPFs have a significant incidence of associated collateral & cruciate ligament injuries which need to be recognised and managed.
Apocryphally, orthopaedic surgeons often describe a fracture as “a soft tissue injury complicated by a break in the bone.” Nowhere is that statement more true than in fractures at either end of the tibia.
A missed popliteal artery injury will have more effect on the outcome for the patient than whatever fracture classification you come up with on the X-ray. Peroneal or other nerve injury is not uncommon; ligament injury or detachment is common and stability significantly affects outcome. Careful examination for neuro-vascular or compartment complications is therefore vital.
However assessment of instability is inhumane before some form of analgesia/anaesthesia, & pointless before fixation of the bone fragments if known ligament ‘attachments’ are in fact detached.
Bennett & Browner, ‘Tibial Plateau Fractures: A Study of Associated Soft Tissue Injuries’; Journal of Orthopaedic Trauma. 8(3):183-188, June 1994. n=30. 17/30 (56%) incidence of soft tissue injuries. Medial collateral ligament in 20%, lateral collateral in 3%, menisci in 20%, peroneal nerve in 3%, anterior cruciate in 10%. Schatzker Types 2 & 4 associated with the most lesions. Type 2 especially associated with MCL injury; menisci commonly affected in Type 4.
Chan et al, ‘Impact of CT Scan on Treatment Plan and Fracture Classification of Tibial Plateau Fractures’. Journal of Orthopaedic Trauma: October 1997 – Volume 11 – Issue 7 – p 484-489. n=21. Addition of CT scans to plain radiographs improved reliability as measured by kappa coefficient. In 26% of cases, it changed the treatment plan.
So now the fracture/ligament injury has been identified, classified, and appropriately treated (easy to find those poorly-evidenced treatment controversies elsewhere, so I won’t go into them here). What about longer term outcomes? I’ll stick mainly with evidence from the last 20-25 years, roughly in chronological order. I recommend obtaining & reading the full papers as soon as you have the time.
Stevens et al, ‘The Long-Term Functional Outcome of Operatively Treated Tibial Plateau Fractures’, Journal of Orthopaedic Trauma: June-July 2001 – Volume 15 – Issue 5 – p 312-320. n=47. Assessment SF-36, & WOMAC. Follow up 8.3 years. Under age 40 NSD between patients & matched control group in SF-36, regardless of fracture type. WOMAC not related to fracture type either (see * regarding classifications above). Over the age of 40, only 12/21 had scores similar to controls. Age at presentation seemed to be the most important factor in outcome. Fracture type had less influence, and adequacy of reduction seemed to be unrelated (!!). The number who had an inadequate reduction was too small to make much of.
Saleh et al, ‘Total Knee Arthroplasty After Open Reduction and Internal Fixation of Fractures of the Tibial Plateau
A MINIMUM FIVE-YEAR FOLLOW-UP STUDY’. JBJS, VOLUME 83-A · NUMBER 8 · AUGUST 2001, 1144-1148.
n=15 consecutive; performed at an average of 38.6 months post-ORIF; 6.2 years follow-up. Assessment = HSSKS, SF-36.
High rate of infection (3); patella tendon disruption (2); & post-operative secondary procedures such as manipulation (3). 3 infection patients required 2 arthrodeses and 1 2-stage exchange.
They commented: On the basis of our results, we concluded that total knee arthroplasty after open reduction and internal fixation of a fracture of the tibial plateau decreases pain and improves knee function, but the procedure is technically demanding and is associated with a high failure rate (five of fifteen).
Weigel & Marsh, ‘High-Energy Fractures of the Tibial Plateau. Knee Function After Longer Follow-up.’ The Journal of Bone & Joint Surgery: September 2002 – Volume 84 – Issue 9 – p 1541-1551. n=31 frax in 30 pts. Minimum 5 years follow-up. No secondary reconstruction surgeries required. Range of Motion ranged 3 degrees extension-120 degrees of flexion (87% of arc of opp knee). 13 rated themselves as excellent; 6 as good; three as fair. 15 were working, including 10 who did heavy labour. PTA on X-ray: 14 = none, 3 = grade 1, 2 =grade 2, 2= grade 3. In most (18) arthrosis had not progessed, although in 4 it had.
Charalambous et al, (Ann R Coll Surg Engl 2007; 89: 400–404. doi 10.1308/003588407X187667) found that the above classifications had high inter-observer variation. Simply classifying into unicondylar or bicondylar and pure splits versus articular cartilage depression +/- split conferred improved inter- and intra-observer variation. Hurrah! (But it would be wise to know Shatzker &/or AO/OTA for an exam anyway, in case the examiner hasn’t read this paper).
Luo et al (”Three-Column Fixation for Complex Tibial Plateau Fractures’. J Orthop Trauma Volume 24, Number 11, November 2010, 683-692) have described a 3-column classification, and surgical approach. I think the concepts advanced in this paper are an important contribution.
Barei et al, (‘Functional Outcomes of Severe Bicondylar Tibial Plateau Fractures Treated with Dual Incisions and Medial and Lateral Plates’, JBJS VOLUME 88-A · NUMBER 8 · AUGUST 2006, 1713-1721). n= M23, F18; follow-up mean 59 months. Assessment by Musculoskeletal Function Assessment (MFA). These authors commented:
Patient age and polytrauma were associated with a higher (worse)
MFA score (p = 0.034 and p = 0.039, respectively). When these variables were accounted for, regression analysis demonstrated that a satisfactory articular reduction was significantly associated with a better MFA score (p = 0.029).
Rank-order fracture severity was also predictive of MFA outcome (p < 0.001). No association was identified between rank-order severity and a satisfactory articular reduction (p = 0.21). The patients in this series demonstrated significant residual dysfunction (p < 0.0001), compared with normative data, with the leisure, employment, and movement MFA domains displaying the worst scores.
Conclusions: Medial and lateral plate stabilization of comminuted bicondylar tibial plateau fractures through medial and lateral surgical approaches is a useful treatment method; however, residual dysfunction is common. Accurate articular reduction was possible in about half of our patients and was associated with better outcomes within the confines of the injury severity.
Brunner et al, ‘Classification systems for tibial plateau fractures; Does computed tomography scanning improve their reliability?’ Injury, Int. J. Care Injured 41 (2010) 173–178. The addition of CT to X-ray evaluation improved intra- & inter-observer reliability to ‘good’.
Manidakis et al, ‘Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases’. International Orthopaedics (SICOT) (2010) 34:565–570
DOI 10.1007/s00264-009-0790-5. n=125/156; 73 males, 52 females. Mean follow-up 20 months. 101 treated surgically, 24 conservatively (usually because of co-morbidity). 15.2% infection. 9.6% residual varus. 8.8% residual valgus. Compartment Syndrome -2. 7 developed DVT ( of whom 3 had PE). 33 (26.4%) had evidence of radiological post-traumatic arthritis (PTA). Severity of injury predicted the later onset of PTA & pain. 5 had required Total Knee Arthroplasty (TKA). The American Knee Society Score (AKSS) was good in 68%, fair in 24%, & poor in 9%.
Malviya, Reed, & Partington. ‘Acute primary total knee arthroplasty for peri-articular knee fractures in patients over 65 years of age.’Injury, Int. J. Care Injured 42 (2011) 1368–1371. n=15 proximal tibia, 11 distal femur. Mean age 80. Mean follow-up 38.8 months. I have to say this is a great paper, because the authors know where I live. The authors said:
Mean Knee Society knee score was 90.2; Knee Society function score was 35.5; Oxford Knee score was 39.5; and Short Form (SF)-36 physical function score was 37.3 and mental score 50.6. Good correlation was noted between Knee society knee score and SF-36 physical function score (Pearson’s 0.76, p = 0.001), suggesting that generic health would dictate the final function achieved, whilst high knee scores suggest the satisfactory results of the operation. Analogous to arthroplasty for hip fractures, this technique should be considered as a treatment option in elderly peri-articular knee fractures with osteoporosis and/or osteoarthritis.
Mehin et al, ‘Endstage arthritis following tibia plateau
fractures: average 10-year follow-up’. Can J Surg, Vol. 55, No. 2, April 2012, 87-94. n=311. 10 year Kaplan-Meier survival analysis for primary outcome of endstage arthritis was 96%; for the secondary outcome measure of surgeries for ‘minor arthritis’ was 87%. The strengths of the study are obviously the hard end-points and the relatively numbers. The main drawbacks of this study are two-fold. Firstly, if latency (time between injury and PTA is over 10 years, the above values will represent only part of the risk (perhaps a small part). Secondly, it depends on the unknown accuracy of multiple coders; linkage between two events; database accuracy issues such as transcription errors, patients going out of state/ changing name etc. The authors go into these issues in more detail.
Ahearn et al, ‘The outcome following fixation of bicondylar tibial plateau fractures’;Bone Joint J 2014;96-B:956–62. doi:10.1302/0301-620X.96B7.
n=55 frax in 54 patients, treated by peri-articular locking plates or limited access internal fixation in combination with a Taylor Spatial Frame. At a minimum of one year patient-reported outcomes showed functional deficits, but no apparent differences between the two modes of treatment. Despite low outcomes scores patients were generally satisfied. The authors said:
We achieved good clinical and radiological outcomes, with low rates of complication. In total, only three patients (5%) had collapse of the joint of > 4 mm, and metaphysis to diaphysis angulation of greater than 5º, and five patients (9%) with displacement of > 4 mm. All patients in our study went on to achieve full union.
This study highlights the serious nature of this injury and generally poor patient-reported outcome measures following surgery, despite treatment by experienced surgeons using modern surgical techniques. Our findings suggest that treatment of complex bicondylar tibial plateau fractures with either a locking plate or a TSF gives similar clinical and radiological outcomes.
Parkkinnen et al, ‘Factors Predicting the Development of Early Osteoarthritis Following Lateral Tibial Plateau
Fractures: Mid-Term Clinical and Radiographic Outcomes of 73 Operatively Treated Patients.’ Scandinavian Journal of Surgery 103: 256–262, 2014. n =73/123. Mean follow-up 54 months. Valgus malalignment of 5 degrees or greater led to more advanced post-traumatic arthritis (PTA) than seen in patients with a normal alignment (p= 0.006). Articular depression >2mm led to more advanced PTA than in patients with less than 2mm (p= 0.001). The degree of malalignment or articular depression had no effect on the WOMAC or Lysholm scores (at this length of follow-up).
Scott et al, ‘Total knee arthroplasty following tibial
plateau fracture’.Bone Joint J 2015;97-B:532–8. n=31, 23F,8M, mean age 65, mean 24 months follow-up. 24 post-ORIF; 7 post-conservative treatment.
Patients with instability or nonunion needed arthroplasty earlier than those with intra-articular malunion. Complication rates higher in PTA TKA than after primary osteoarthritis. Wound complications 13% -v- 1%. Persistent stiffness 10% -v- 0%. 6% revision TKA at 57 & 114 months. No significant difference in post-op Oxford Knee Score or patient satisfaction, (although the primary osteoarthritis group had had worse pre-operative scores to start with).
The authors said:
Total knee arthroplasty undertaken after fracture of the tibial plateau has a higher rate of complications than that undertaken for primary osteoarthritis, but patient-reported outcomes and satisfaction are comparable.
Kraus et al, ‘Duration of incapacity of work after tibial
plateau fracture is affected by work
intensity’. BMC Musculoskeletal Disorders (2018) 19:281
https://doi.org/10.1186/s12891-018-2209-1.
n=39; ages 20-61; minimum follow-up 14 months. The authors found:
The median incapacity of work was 120 days (range 10–700 days) with no significant differences between B- and C-type fractures.
Four (10.3%) patients reduced their working hours by 10.5 h per week on average. Patients with low workload (REFA 0–1, median incapacity of work 90 days, range 10–390 days) had a significant shorter incapacity of work than patients with heavy workload (REFA 2–4, median incapacity of work 180 days, range 90–700 days) (p < 0.05). The median Lysholm score decreased significantly from 100 points (range 69–100) before the injury to 73 points (range 23–100) at the time of the follow-up. All patients received postoperative physiotherapy (median 25 appointments, range 6–330), with a significant higher number of appointments for C-type-fractures than for B-type-fractures (p = 0.004).
Conclusion: A relationship was found between workload and the duration of incapacity of work after tibial plateau
fractures. The post-injury shift to less demanding jobs and the reduction of working hours highlight the impact of a tibial plateau fracture on a patient’s subsequent physical ability to work.
Biz et al, ‘Challenging Surgical Treatment of Displaced
Articular Tibial Plateau Fractures: Do Early Knee
Radiographic Features Have a Predictive Value of
the Mid-Term Clinical Functional Outcomes?’Orthopaedic Surgery 2019;11:1149–1162 • DOI: 10.1111/os.12577.
n=45; 29M, 16F. Follow-up mean 57 months.
The authors noted: ‘There were AO 41-B fractures (partial articular fractures) in more than half of the patients (66.67%), while the remaining 15 had AO 41-C fractures (complete articular fractures). The sub-type AO 41-B3 was the most common, reported in 62.22% of patients. The mean KOOS score was 69.0. Mean AKSS and SF- 36 PCS scores were 79.0 and 41.4, respectively. There were significant relationships between age and functional results (KOOS ADL, Sport, QoL, and SF-36 PCS) and between BMI and KOOS Pain, ADL, Sport, and QoL. No differences were found between the two types of fractures regarding quality of reduction and alignment. AO 41-C TPF tend to develop PTOA more frequently with respect to 41-B fractures, while type AO 41-C TPF had the worst clinical outcomes.
We found that the presence of an articular step-off and the malalignment of the tibial axis after surgery were predictive of daily pain felt by patients. PTOA was predictive of a worse AKSS. The overall complication rate was 13.33%: 1 superficial wound infection, 1 deep vein thrombosis, and 4 cases of transitory deficit of the common peroneal nerve.
Conclusion: The present study demonstrates that early radiographic features may be predictive for pain perceived by patients at mid-term follow-up.‘
Larsen et al, ‘Patient-reported and Functional Outcomes of Bicondylar Tibial Plateau Fractures Managed by Internal Screw Fixation in Combination with An Ilizarov Fixator: A Case Series of 22 Patients with Long-term Follow-up’.Strategies in Trauma and Limb Reconstruction (2019): 10.5005/jp-journals-10080-1432.
n=22, 14M, 8F. Mean 9.4 years follow-up.
‘The mean knee injury and osteoarthritis outcome score (KOOS) was pain 72.5, symptoms 62.7, ADL 75.9, sport 35.4, and knee related quality of life (QOL) 56.4. Compared to a reference population, the present study reported worse outcome for the subscales: symptoms, sport, and QOL. The maximal isometric muscle strength for knee extension was 354N for the noninjured leg and 325N for the injured leg (p = 0.27). Assessment of gait functions showed a gait speed of 122.7 cm/second and a cadence of 112.7 steps/minute. Gait speed and cadence showed no significant difference when compared to a reference population. Radiological examination of knee osteoarthritis (OA) showed 6 patients presented with none OA, 13 patients with mild OA, and 3 patients with severe OA.
Conclusion: Complex bicondylar tibial plateau fractures are associated with long-term decreased knee structure-specific patient-reported
outcome (KOOS). In contrast, most patients presented with satisfactory long-term radiological and functional outcomes.’
Gonzalez et al. ‘Patient function continues to improve over the first five years following tibial plateau fracture managed by open reduction and internal fixation’. Bone Joint J. 2020; 102-B(5): 632-637
n=102 displaced tibial plateau fractures, operatively treated. Assessment: Visual Analogue Scale (VAS) or Numeric Rating Scale (NRS) pain scores, Short Musculoskeletal Functional Assessment (SMFA), and knee range of movement (ROM).
The authors noted the following results: ‘Patient-reported functional outcomes as assessed by overall SMFA were statistically significantly improved at five years (p < 0.001) compared with one-year data from the same patients. Patients additionally reported an improvement in the Standardized Mobility Index
(p < 0.001), Standardized Emotional Index (p < 0.001), as well as improvement in Standardized Bothersome Index (p = 0.003) between the first year and latest follow-up. Patient reported pain and knee ROM were similar at five years to their one-year follow-up. In total, 15 of the patients had undergone subsequent orthopaedic surgery for their knees at the
time of most recent follow-up. Of note, only one patient had undergone knee arthroplasty following plateau fixation related to post-traumatic osteoarthritis (OA).
They summarized: ‘Knee pain following tibial plateau fracture stabilizes at one year. However, patient-reported outcomes continue to improve beyond one year following tibial plateau fracture, at least in a statistical sense, if not also clinically. Patients displayed statistical improvement across nearly all SMFA index scores at their minimum five-year follow-up compared with their one-year follow-up’.
Summary:
- undisplaced & minimally displaced injuries do well
- displaced fractures that need surgical intervention do well provided: complications are avoided, the joint surface can be restored & maintained, union can be obtained, ligament stability is achieved, & limb alignment is maintained within 5 degrees
- pain following plateau fracture stabilises at one year; other patient-reported outcome measures continue to improve for 5 years (presumably excepting the ~15% who required further surgery in Gonzalez’s paper.
- It is common for there to be limitations in relation to sport and heavy work, whether that is in employment or at home
- Ultimately, damage to joint surfaces may lead to post-traumatic arthritis in some
- total knee arthroplasty is a reasonable solution for PTA, or in the un-reconstructible fracture in an elderly patient. There is a higher complication rate in this setting, when compared to primary arthroplasty for OA